Written by: Lee Thomas
Time to read: 8 minutes
Note: Many Aleo blog posts are meant to be read by clients who are struggling with disordered eating or body image concerns. This one, though, is specifically for clinicians. (But of course anyone is welcome to read it!)
In my therapy practice, many people I work with have sought me out specifically because of my eating disorder specialization, which is probably not super surprising. Want therapy for an eating disorder, see an eating disorder therapist.
But a lot of clients I’ve worked with over the years didn’t come in initially for eating disorder therapy. They came in for other concerns — alcohol use, relationship problems, childhood trauma, work stress, ADHD management, you name it — and then in our work together we discovered that they have a disordered relationship with food. My secret strategy for uncovering this? I ask.
“What is your relationship with food?” is a pretty standard question for me to ask within the first session or two. If the client answers in a way that suggests a disordered relationship with food, usually my followup question is “have you ever talked about this with a therapist before?” What I’ve found surprising is that the answer is almost always no… even when it’s a client who had already been in therapy for many years.
Now, to be clear, this isn’t meant to be a shaming “gotcha!” to you or any other clinician. Clinicians are fallible, myself included. We all bring our own lenses into this work — and we don’t tend to find what we’re not looking for.
“I don’t work with eating disorders” is a common thing for me to hear therapists say. But this creates a vicious cycle where clinicians believe they don’t work with clients with eating disorders, and so don’t ask their clients questions about eating disorders, and so they don’t hear about their clients’ eating disorders, and so they continue to believe that they don’t work with clients with eating disorders.
And obviously nobody is required to change their practice in any way just because I wrote a blog post. But what I’m hoping to do here is to help clinicians recognize that 1) yes, you can work with clients with eating disorders, and 2) you don’t have to do it alone.
To start with, let’s name some concerns that you, as a clinician, might have about working with clients with eating disorders.
“I need to work through my own food stuff first!”
You might have your own disordered relationship with eating and not feel like you’re in a place where they can effectively work with others around this topic. Even though you’re a clinician, you are a person first, and it’s absolutely okay to be selective about your work in order to keep yourself well. That being said, I don’t think your own disordered relationship with food inherently precludes you from being a good therapist to others. My own early work in the mental health field was as a “person with lived experience” (as we called it back then), and there’s lots of good work by Dr. Jennie Wang-Hall on this topic as well. Having support through something like a clinical consultation group can help you to explore things like countertransference to help ensure you’re taking care of both yourself and your clients.
“Clients with eating disorders don’t want to change.”
There’s still, unfortunately, a lot of stigma around people with eating disorders. Clients with eating disorders are still sometimes portrayed as manipulative, untrustworthy, unmotivated, and resistant. Can they be those things? Sure. They are human beings. We are all capable of being those things, sometimes. But a lot of this stigma is based on carceral beliefs about mental health care provision, and it’s not true.
In defence of most clinicians, in my experience the percentage of clinicians who don’t work with clients with eating disorders because of overt stigma is actually pretty low. (Or maybe that’s the circles I run in, because the research definitely reflects that stigma is still very much present.) But none of us are infallible, and it can be easy to slip into stigmatizing beliefs if you’re not surrounded by a community of clinicians who can support you when you’re feeling discouraged, and lovingly hold you accountable when you start to veer off course.
“There’s too many liability concerns.”
I’ve been in a lot of clinician consultation groups, and a common thread that I hear is that we as clinicians are terrified of getting in trouble, whether that’s with our college or with the legal system. In a lot of ways this can be a good thing — we have a lot of power in the therapeutic relationship, and having the college as an institution to protect the public helps to ensure that health care professionals are behaving ethically. However, I do think that sometimes the fear of getting in trouble becomes a sort of boogeyman that causes clinicians to be more risk averse than is necessary, even when it’s to the client’s detriment. We’re so afraid of doing the wrong thing so we end up doing nothing! And eating disorders can exacerbate this risk aversion because of the physical health concerns involved. Part of the benefit of a consultation group is that you can explore your concerns with other professionals, who can help you to figure out which risks feel worthwhile.
“It’s outside of my scope.”
I think there’s a both/and to be had here. On the one hand, it’s really important to practice within our scope and training. Like, I don’t have any EMDR training, so it would be wildly unethical if I were to just start doing EMDR (especially if my only motivation was that some random person wrote a blog post telling me that I should). But on the other hand, I think it’s also important to acknowledge that part of how we expand our scope is by pushing into new areas where we are not yet an expert.
I think this is especially true for clients where you already have an established relationship. Research consistently shows that the biggest predictor of positive therapeutic outcomes is the relationship between the client and the clinician. You might not be an eating disorder expert, but you might be a Therapeutic Alliance With This Specific Client expert, and that’s a really, really important element to consider. If you’re considering expanding your scope in order to support an existing client, consultation (whether individual or group) is definitely something you’ll want to pursue to help you increase your clinical skills and steer clear of potential pitfalls.
“I only work with trauma (or anxiety, or substance use, or…)”
This is a variation of the “scope” concern, I think. And, again, if you really want to stay in your specific wheelhouse, nobody is stopping you. But there’s a ton of comorbidity with eating disorders and other conditions. If you’re working with trauma, or anxiety, or substance use, or almost any other area, you are almost certainly also working with clients with eating disorders. And that’s even before we consider the subthreshold eating disorders, aka disordered eating. Food is one of the basic building blocks of the human experience — it’s going to influence, and be influenced by, other conditions in a client’s life. If someone has experienced trauma we aren’t shocked when it impacts their relationship with romantic partners, friends, work, or many other elements of their life. We should expect that it would impact their relationship with food, too.
So all of this to say: the reality is that you’re already working with clients with eating disorders. The choice you have now is what you want to do with this information.
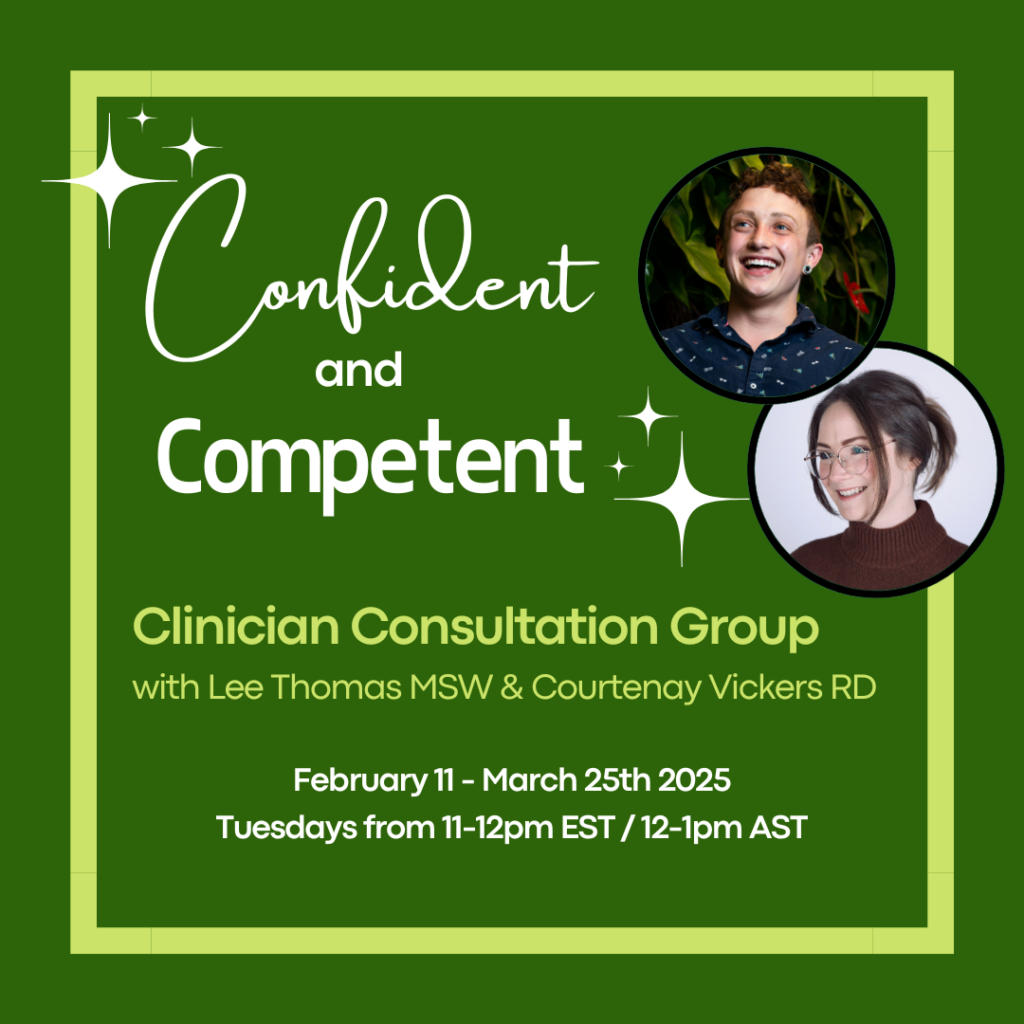
If you’re open to suggestions, I think the Confident and Competent Clinician Consultation Group could be a good place to start.
As a clinician in a private practice, I’ve made a point of investing in consultation throughout my career, and I truly can’t overstate the impact that it’s had on my practice. A consultation group is a soft place to land when you’re feeling discouraged, and it’s a reality check when you’re way off track. It’s a place to learn strategies and phrases that your colleagues find helpful with their clients. It’s a source of reassurance and guidance. And, as a bonus, it’s often counted as continuing education credits.
Courtenay Vickers is a registered dietitian and member of the Aleo Collective. She and I decided to start this group because we’ve both found consultation to be unbelievably valuable to ourselves, our practices, and our clients — and we want to share it with you!
Registration for our group closes January 31, 2025. We would love for you to join us!