Written by: Lee Thomas
Time to read: 10 minutes
Note: This blog post contains descriptions of disordered eating behaviours. A content warning is listed prior to that section.
When it comes to eating disorders, there is no shortage of fighting imagery. Beat it, conquer it, destroy it, defeat it. And before you read another word here, I first want to say: if those approaches work for you, or your loved one, or your client? Then keep doing them. I’m not trying to take this from you.
But for a lot of people, this approach isn’t working.
We know that many people never get treatment. And for those who do, they often don’t complete treatment. And even for those who do, there is a high rate of “relapse.” There’s no universally agreed-upon definition of recovery or relapse, so articles vary wildly in the numbers they quote, but everyone seems to agree that eating disorders are often a long-term struggle.
So, clearly, something isn’t working here. But why?
Maybe it’s because the eating disorder isn’t actually evil.
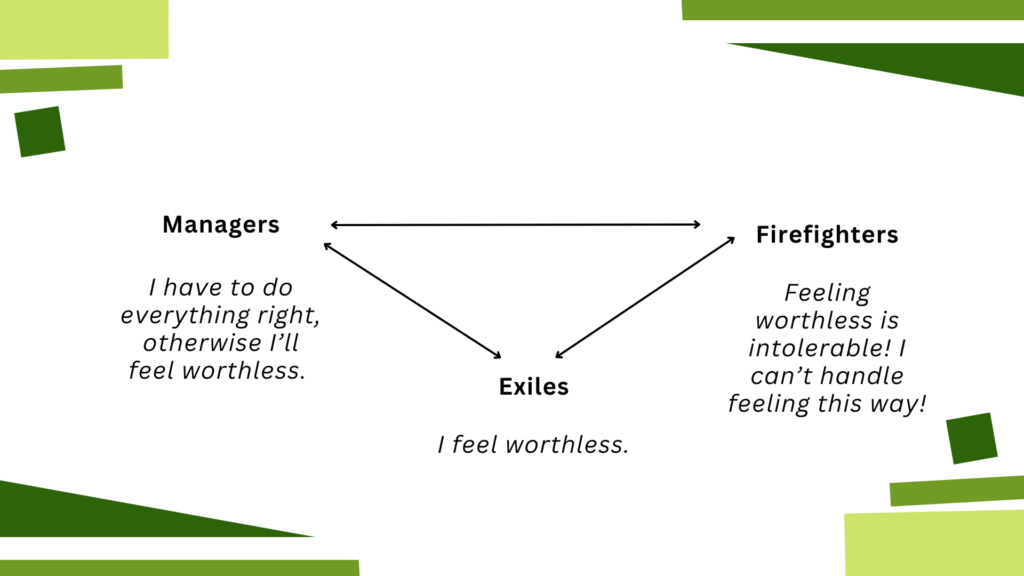
Enter IFS, stage left. Internal Family Systems therapy, or IFS, is based on the concept of multiplicity — that your mind isn’t all one thing, even though that’s what you’ve probably been taught most of your life. Instead, your mind is made up of a bunch of different subpersonalities, or “parts.” Sort of like the movie Inside Out, but for real. In IFS we divide these parts into 3 categories:
Exiles are generally young parts of us that hold a lot of big emotions, especially pain. This might be the part of us that says “I feel worthless”.
Managers are the proactive parts of us that try to prevent this exiled pain from overwhelming us. This might be the part of us that says “I have to do everything perfectly, otherwise I’ll feel worthless.”
Firefighters are the reactive parts of us that leap into action when the exiled pain is overwhelming us. This might be the part of us that says “I can’t handle feeling this way! I have to make it stop!” And will do whatever it takes to rescue us in that moment.
[Content warning: disordered behaviours. Skip this italicized section if you’d like to avoid]
In real life, this might look something like this: I might have an exile that believes that my body is bad and wrong, and feels a ton of shame whenever anything body-related comes up. In order to prevent this shame from flooding me, I might have a manager that says “if you just lose weight, then you won’t need to feel that shame.” And maybe it works, for a moment…
…But then, maybe I am rejected by a potential romantic partner, and I assume (rightly or wrongly) that it’s because of my body. The exile comes screaming out and starts to flood me with feelings of shame. It’s like an emotional fire that’s burning me up inside. It feels intolerable. So then a firefighter comes in to rescue me from this fire, and I scramble to the cupboard to eat anything I can get my hands on, whatever it takes to numb this horrible feeling. And maybe it works, for a moment…
…But then the manager voice comes back online and is horrified and critical: “I can’t believe you ate all of that! You’re disgusting! You’re a failure! No wonder nobody likes you!” This makes my exile start to feel shame again, and a firefighter comes back in to put out this new fire: get rid of the food. And maybe it works, for a moment…
…But then the manager criticizes me for throwing up and pledges that tomorrow we won’t let ourselves eat so much, because that’ll make up for today being such a disaster. And on, and on, and on.
So as you can see, the parts are trying desperately to help keep things stable in their own way — even though the ways in which they’re trying to help aren’t, in fact, helpful. Like many elements of disordered eating, it’s like being stranded in the middle of the ocean on a raft and drinking salt water to try to quench your thirst, even though it ultimately makes you more dehydrated. It’s an act of desperation that, despite being unhelpful in the long term, is entirely understandable given the circumstances. And, despite being entirely understandable given the circumstances, is also not helpful long term. Just because it hurts doesn’t mean it’s malicious, and just because it’s not malicious doesn’t mean it doesn’t hurt.
There’s another element at play as well, something that’s not exactly a part — your Self. One of the things that I like about IFS is also one of the things that I have struggled with the most about it, which is that it is unabashedly spiritual. IFS believes that everyone has a Self, which is sort of like a soul, or a core You.
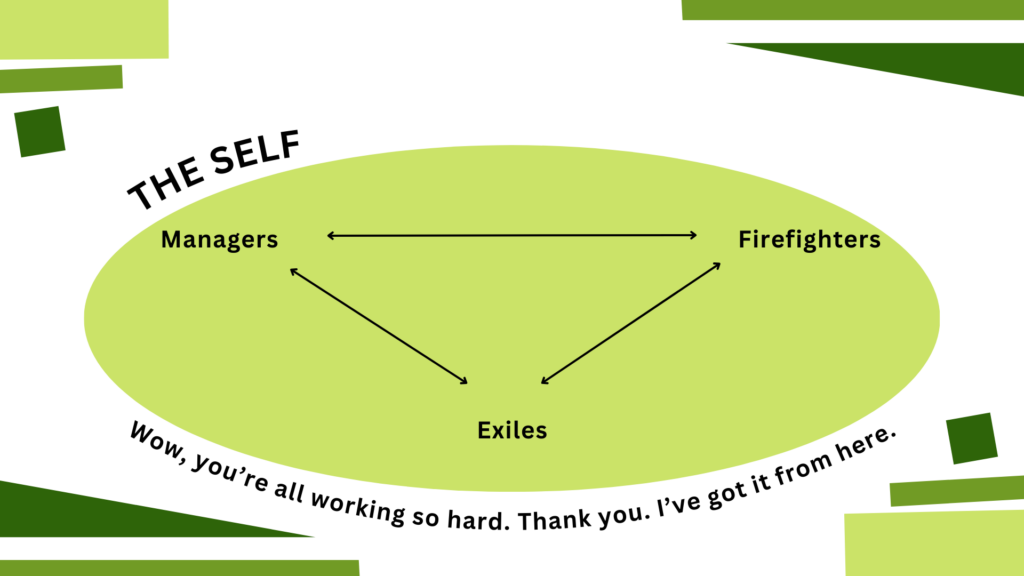
This Self is like a compassionate, curious, loving parent figure. It knows that your parts are trying so hard to help you, that they actually kind of hate the job that they’re doing right now, and that they’re only doing it because they feel like they have to. We say there are No Bad Parts because the parts aren’t evil or malicious. They’re just extremely misguided. They are so good in their hearts, they are trying so hard to help, but they have very hard, and sometimes very harmful, jobs.
In our italicized example above, the exile part is holding onto so much pain related to shaming experiences around my body. The manager part wants to help prevent this pain, so they criticize me harshly before anyone else gets a chance to, even though they know it’s hurtful. The firefighter part doesn’t want to see me incapacitated by pain, so they try to help using the only tools available to them, even though this job earns them nothing but criticism from all the other parts (not to mention everyone else in my life). These parts are so profoundly dedicated to helping me, even at the expense of their own wellbeing. So then when outsiders like therapists and family members label these parts as “monsters” and “enemies,” no wonder they push back.
So if we’re not fighting them, what do we do instead?
It’s not easy, but it is simple. We love them.
If you rolled your eyes here, I feel you. There’s a part of me that genuinely can’t believe the type of therapist I am now. I can hear my younger self saying incredulously, “A key component to healing from an eating disorder is love? Grow up.” But unfortunately, it is true. I sometimes joke that I became an IFS therapist because at my heart I’m actually an ACT therapist — it’s all about workability for me, and this loving approach works.**
At its heart, IFS is about building community. Imagine if you felt like you belonged, and were safe, and unconditionally cared for. Imagine the sort of healing you could do if you felt like you were deeply loved no matter what. Imagine if someone saw the good in you even when you yourself can’t see it. That’s the power of community. IFS helps you to create that world internally, which can help you create it externally, too.
So what does that look like in real life?***
I might have an exile that feels a huge amount of shame about my body. I might work with this exile in therapy to help it to release the beliefs that burden it. I might help it get un-stuck from the past. I might let this exile know that I’m delighted by it, and that not only am I able to take care of them, but in fact I would be thrilled to take care of them.
I might have a manager that says “if you just lose weight, then you won’t need to feel that shame.” And I might sit with that manager and say “It makes so much sense to me that you feel that way. Thank you so much for trying to protect me.” I might help that manager to understand that I’m not a little kid any more, that they don’t need to take care of me. I might let this manager see that I care about my future and that they don’t need to be harsh in order for us all to be safe.
If my exile gets triggered and my firefighter comes in to rescue me, I might say “Wow. You are working so hard. Thank you so much. I’ve got it from here. I love that exile part, and its distress isn’t too much for me to handle.” I might let the firefighter see that I’m still engaging in pleasurable activities even when things aren’t on fire. I might tell them how much I appreciate all the things they’ve done to try to protect me over the years.
I do want to reiterate that being compassionate doesn’t mean that we’re enabling these parts. Loving a child doesn’t mean that we let them drive the car. But it does mean that we respond to them with compassion and kindness rather than with cruelty and punishment. We’re not fighting them because they’re not our enemy. We appreciate how hard they’re trying to help, and we recognize that they’ve been trying to help us for a long, long time. As Sam Dylan Finch wrote in this excellent blog post, “To relate to my ED as something I have to ‘fight’ or ‘beat’ is a betrayal of all the younger versions of me that conspired to protect my life and my future. I wouldn’t be here without them.”
Our parts love us deeply, and it’s about time we love them back.
If you’re interested in working with an IFS therapist, I recommend using the IFS directory or searching out someone who has received a minimum of Level 1 training from the IFS Institute. As of the time of writing this article I am not currently accepting new clients for individual therapy, but you’re always welcome to check my availability here to see if that’s changed. I do have spots available for clinical consultation.
* For the record, I think that the blog post on externalization that I pulled this quote from was very thoughtful and well-done, so I don’t mean for this to be perceived as a criticism of the blog post itself
** IFS is not a new therapy, but it is having a very hot moment right now, so lots of people are hearing about it. In some ways, I love this — I think IFS is great, and I have personally and professionally experienced how powerful it can be. But I feel like it’d be remiss not to note that so many therapies have had this same arc. Therapeutic modalities can be trendy just like anything else. So do I think IFS is amazing and a therapeutic modality well worth considering? 100%. But do I think it’s a perfect panacea and the only possible route to healing? Absolutely not.
*** If these examples sound trite or corny, I get that. Taking this stuff out of the individual therapeutic context has that effect, but I felt like I should include some examples anyway. Please trust me when I say that if you do this work with your own parts, the compassionate statements you come up with will not feel corny at all.