Written by: Dustin LindenSmith
Time to read: 12 minutes
Please allow me to introduce myself: I go by Dustin, my pronouns are he/him, and I’m grateful to live with my wife and three children on a lake situated on the unceded ancestral territory of Mi’kmaqi and the Mi’kmaq people, at Punamu’kwati’jk (”Boonamagwaddy”), known in modern times by its colonialist name of Dartmouth, Nova Scotia (across the harbour from Kjipuktuk (Chebucto), now known as Halifax). I am a White, cisgender man, a stay-at-home dad, a jazz musician, a recovering IT professional, and a peer supporter for people in recovery from eating disorders. I am also currently studying for my Master’s in Counselling Psychology to become a psychotherapist.
I come to this work by way of my own lived experience and my ongoing recovery from childhood trauma and an eating disorder.1 I first started eating for emotional comfort and stress relief at age 7, and I was always known as a “husky” child. I went on my first weight-loss diet in my pre-teens, and by the time I reached high school, I had “dieted my way up to” a very high weight. After another couple of weight-loss cycles followed by longer periods of weight gain, I became very fat by the halfway point of my undergraduate degree. I would go through about eight large swings of weight-cycling from that point until I entered recovery some 30 years later.
What I needed to recover from was an eating disorder. When I entered recovery, I estimated that I had gained and lost the equivalent of four times my adult body weight throughout my life—truly an epic, lifelong cycle of yo-yo dieting. Once I really connected the dots between my childhood trauma and my decades-long, food-based emotional coping habits, I was finally able to stop my weight-cycling behaviours by never starting another weight-loss diet again. However, in the fatphobic, diet-obsessed culture we live in, refusing to go on a diet is itself a quasi-revolutionary, countercultural act.
SOTU (State of the Union) for Fat People Today
First, a word about the word “fat”. People “of size” are reclaiming the word fat as a simple descriptor for our bodies that is stripped of its usual negative and pathologizing connotations. I will use the word as a non-judgmental reference term for people like me who live in larger bodies, and whenever I use the word, I do not imply that there is anything inherently wrong or unhealthy about merely being fat.
Second, our status: our numbers seem to be increasing every year, with the causes being multifactorial, complex, and interrelated with one’s socio-economic, cultural, and intersectional positioning within their community. In healthcare, the medical community certainly treats obesity as inherently pathological, but there is no consensus on how to “solve the problem of obesity” or even how to clearly define what “the problem” is in the first place (recent pharmaceutical developments with GLP-1 inhibitors such as Ozempic notwithstanding).
Third, how fat people might present today is multifaceted, but many of us share similar backgrounds and experiences. For years—likely dating back to our childhoods—many of us have had a dysregulated relationship with food, movement, and our bodies. Many of us have experienced chronic and severe weight cycling throughout our lives as a result of chronic weight-loss dieting, and many of us have experienced adverse childhood experiences that involved trauma, neglect, or abuse. Once more for the people in the back: Fat people are themselves often survivors of trauma and abuse.
A Primer on Anti-Fat Bias and Toxic Diet Culture
Anti-fat bias is rampant in our culture, and it is a force which is colonialist, misogynist, and racist in origin. It arises from holdover imperialist ideas about man’s apparent dominion over our mind and our bodies, and of mind over matter. It clings to the ill-conceived notion that we should all be capable of keeping the body “in line” through the rigours of our own mind and willpower, and this has cultivated a learned distrust within ourselves about our bodies. Many of us have lost faith in our own judgment about what is “the right thing” to do for our bodies.
Fat stigma is shot through our families, popular culture, our society, and in our physical spaces (e.g. restaurants, airplanes, and public seating areas which cannot comfortably accommodate fat people). In healthcare settings, it shows itself through the relentless pursuit of thinness for its own sake (+ the inanity of considering one’s BMI on its own as a diagnostic indicator for anything clinically useful on its own merits). We are also all involved (willingly or not) in a multi-billion-dollar dieting and weight loss industry that is deeply pervasive in our popular culture, news and social media, and within many of our friends and family groups.
Why Are We Fat, Anyway?
With apologies to any medical folks in the crowd, I’d like to start with a disavowal of our collective and cultural drive to be thin in the first place. It is simply not necessary to be thin in order to be happy or healthy, and just like anyone else, fat people deserve to be loved and to feel joy.
There are also well-established links between trauma, adverse childhood experiences (ACEs), and disordered eating behaviours 2. Some of us have that history + a personality type or an entrenched pattern of behaviour that derives emotional comfort or stress relief from eating or overeating, and this has led to weight gain over time.
Dieting for weight loss also contains a painful, intrinsic paradox: people can easily become fat by dieting for weight loss. Dieting has a 95+% failure rate for long-term, sustainable weight loss because of how our biology thwarts long-term weight-loss due to its protective metabolic functions against famine and starvation2. There is almost always an unhealthy rebound effect with dieting and weight-cycling, which can best be described as the result of a restrict*-then*-binge cycle (and not a binge-then-restrict cycle—i.e., the restricting comes first).
Being fat in this culture also brings with it body shame, self-loathing, a lack of self-trust, and pervasive feelings of failure and worthlessness resulting from years of “failing” at weight-loss diets. Shame is a physical manifestation of the existential fear that we might become excluded from our group, and this can often lead to dysfunctional and maladaptive behaviours and relational patterns3.
Many of us also deprive ourselves of food (and/or we have an adversarial relationship with it), and this can result in caloric restriction which then incites binge-eating behaviours. The truth is, *we all deserve to eat—*but not all of us believe that we deserve to eat (and/or not all of us believe that we deserve to eat what we want to eat and when we want to eat it).
In my observation, there are also certain factors that do not usually contribute to our fatness: these are a lack of self-insight, a lack of awareness, a lack of motivation, a lack of information, or a lack of knowledge. What we are missing is something much different than those things.
So What Do We Do Now?
So far, I’ve set some of the context for what it’s really like for fat people to live in a fatphobic world. But what can really do about all of that? I have four concrete things to suggest: (1) changing the way we think (and act) about fatness and our bodies; (2) cleaning up our social media feeds; (3) working on our boundaries; and (4) seeking professional support to work with any or all of the above.
Let’s get into each one in some detail.
1. Changing the way we think (and act) about fatness and our bodies
Here are some ways we can start to adjust our mindset and self-view about our own fatness and how we deserve to show up in the world.
- cultivating accurate empathy and self-acceptance towards ourselves by working with our shame and forgiving ourselves for our past behaviour with food and movement
- acknowledging our inherent sense of goodness and self-worth: acknowledging that we are all perfectly good, worthy people and we deserve to exist, to eat, and to take up space in this world—no matter what size we are or what number comes up when we step on a scale or whether we think “society” finds us attractive or whether we’ll find a partner or have a family
- personal self-development and embodiment work: practicing personal self-development work that gets us into our bodies and cultivates mindfulness and self-acceptance (e.g. journaling, art, writing, crafting, singing, dancing, playing, music, acting, movement, or other embodiment exercises such as sports, yoga, tai chi, swimming, strength training, martial arts, walking, working out, golfing, racquet sports, sports in the water, hiking, camping, bouldering, landscaping, and more)
- radical self-love: learning how to transform our adversarial relationship with our bodies into what Sonya Renee Taylor calls radical self-love
2. Cleaning up our social media feeds
Extensive research has confirmed that the use of social media has been linked to various poor mental health outcomes (e.g., Gioia et al., 2020; Keles et al., 2020). Here are some suggestions for how to mitigate those harms for yourself:
- acknowledge SM’s real potential harms to our self-image, body image, and self-worth when we drench ourselves in comparisons with the beauty and health content online
- initiate some accurate (but compassionate!) self-inquiry about your usage habits and about what you really want to “get” from your social media (e.g., if it’s for entertainment but the end result is that the images you’re exposing yourself to are harming you and making you feel terrible about yourself, is it really giving you what you’re looking for?)
- revisiting privacy settings, posting/reading frequency, screen time settings
- unfollowing accounts focused on weight loss, dieting, “clean” eating, excessive exercise, and anything that otherwise appears to promote toxic diet culture or misogynistic beauty standards
- adding new accounts that pass your new fat-positive vibe check (e.g., the beautiful Black yogini Jessamyn Stanley (@mynameisjessamyn) (and don’t miss this guest reel by @funkingafter50); the ineffably happy Toronto gay bear Lukas (@bearlyfriendly); and the photographer and artist Sugar McD (@shooglet), who has taken some of the most beautiful pictures of fat people experiencing joy that I have ever seen)
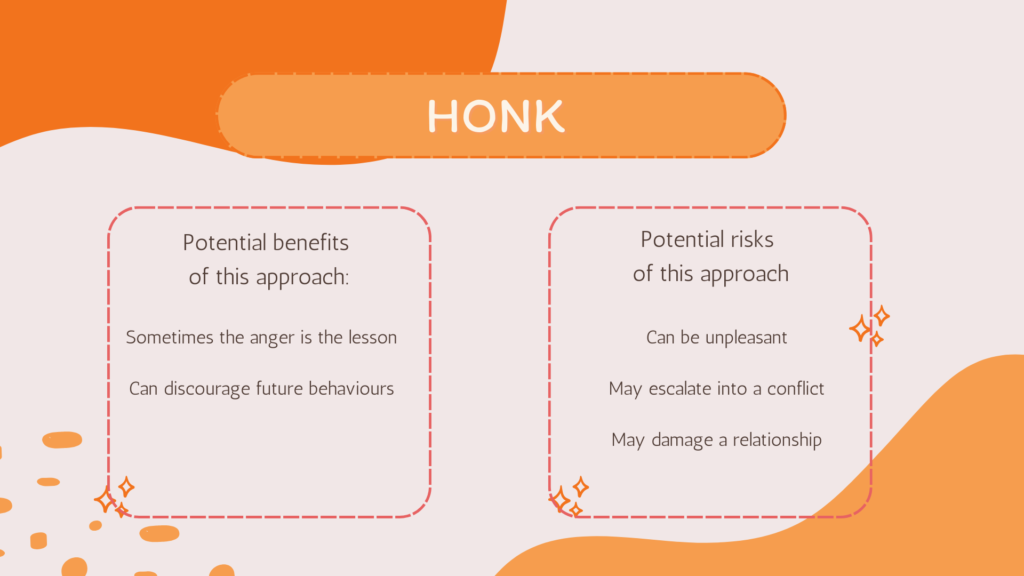
3. Working on boundaries
This is the one I have personally found the most difficult; throughout my entire life, I have pre-emptively made self-deprecating fat jokes about myself in social settings in a misguided attempt to make everyone comfortable. I now understand that this habit was causing me more harm than I knew, and it was also giving everyone in my life implicit license to speak disrespectfully about my own weight.
It takes real courage (along with possibly a previously-unknown self-respect) to build up the confidence to start the challenging but worthwhile work of informing the people in your life that you’re no longer willing to put up with a certain type of discussion or judgment about your body weight, your diet, your food choices, or your health.
The best introduction to the topic I can suggest is Aleo’s own Lee Thomas’s 2-part blog post on this topic. When you’re ready to go deeper, I recommend looking at Black psychotherapist Nedra Glover Tawwab’s excellent work (e.g., her website, her Instagram, her book, and her workbook are all excellent resources).
4. Professional support
One of the sweetest gifts you can give yourself is the gift of professional support for what you’re struggling with. If you want to take a fresh new approach to your recovery, working with anti-diet, anti-oppressive practitioners such as the ones you will find at The Aleo Collective would be a great start. Lee and Raquel are MSWs; Courtenay is a Registered Dietitian, and I am a Peer Supporter who works with people in recovery from disordered eating and self-image issues.
References
American Psychiatric Association [APA]. (2022). Diagnostic and Statistical Manual of Mental Disorders, 5th ed., text rev. (DSM-5-TR). https://doi.org/10.1176/appi.books.9780890425787
Bakalar, J. L., Barmine, M., Druskin, L., Olsen, C. H., Quinlan, J., Sbrocco, T., & Tanofsky‐Kraff, M. (2018). Childhood adverse life events, disordered eating, and body mass index in US Military service members. International Journal of Eating Disorders, 51(5), 465–469. https://doi.org/10.1002/eat.22851
Brewerton, T. D. (2022). Mechanisms by which adverse childhood experiences, other traumas and PTSD influence the health and well-being of individuals with eating disorders throughout the life span. 1–20. https://doi.org/10.1186/s40337-022-00696-6
Doran, J., & Lewis, C. A. (2012). Components of Shame and Eating Disturbance Among Clinical and Non-clinical Populations: Shame and Eating Disturbance. European Eating Disorders Review, 20(4), 265–270. https://doi.org/10.1002/erv.1142
Freire, R. (2020). Scientific evidence of diets for weight loss: Different macronutrient composition, intermittent fasting, and popular diets. Nutrition, 69, 110549. https://doi.org/10.1016/j.nut.2019.07.001
Gioia, F., Griffiths, M. D., & Boursier, V. (2020). Adolescents’ Body Shame and Social Networking Sites: The Mediating Effect of Body Image Control in Photos. Sex Roles, 83(11–12), 773–785. https://doi.org/10.1007/s11199-020-01142-0
Hemmingsson, E., Johansson, K., & Reynisdottir, S. (2014). Effects of childhood abuse on adult obesity: A systematic review and meta-analysis. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity, 15(11), 882–893. https://doi.org/10.1111/obr.12216
Keles, B., McCrae, N., & Grealish, A. (2020). A systematic review: The influence of social media on depression, anxiety and psychological distress in adolescents. International Journal of Adolescence and Youth, 25(1), 79–93. https://doi.org/10.1080/02673843.2019.1590851
Noll, S. M., & Fredrickson, B. L. (1998). A Mediational Model Linking Self-Objectification, Body Shame, and Disordered Eating. Psychology of Women Quarterly, 22(4), 623–636. https://doi.org/10.1111/j.1471-6402.1998.tb00181.x
Schiff, M., Helton, J., & Fu, J. (2021). Adverse childhood experiences and obesity over time. Public Health Nutrition, 24(11), 3205–3209. https://doi.org/10.1017/S1368980021001804
Spreckley, M., Seidell, J., & Halberstadt, J. (2021). Perspectives into the experience of successful, substantial long-term weight-loss maintenance: A systematic review. International Journal of Qualitative Studies on Health and Well-Being, 16(1), 1862481. https://doi.org/10.1080/17482631.2020.1862481